Case 5 – Evaluating a patient with C2-C3 facet joint dysfunction (Preview)
Disclaimer: Please read the Disclaimer at the bottom of this page.
Copyright © Educom Pty Ltd: All material on this website (including the text, graphics, videos and downloadable files) are owned by or licensed to Educom Pty Ltd and is subject to copyright and other intellectual property rights under international conventions.
A Problem-Solving Approach to History Taking and Physical Examination
The learning material in this unit is designed to improve your skills in history taking and physical examination. The material includes examples of clinical findings and their analysis using a problem-solving approach. As you read through the material and watch the videos, you are encouraged to identify whether all the required elements of history taking and physical examination have been adequately covered.
Taking the Patient’s History
When taking the patient’s history, the practitioner needs to obtain sufficient information to cover the following essential elements:
• Who is the patient?
• Where is the pain?
• When was the onset?
• What caused the onset?
• What are the pain characteristics?
• What are the aggravating and relieving factors?
• What has been the course of the pain?
• Are there any associated symptoms?
• Is there a past history that is relevant to the current complaint?
• Are there any “red flags”?
• What is the list of possible causes for the patient’s complaint?
Who is the patient and where is the pain?
When was the onset and what caused the onset?
Your patient is a 67-year-old company director who presents complaining of right upper posterior neck pain. He says that the neck pain began after he attended a meeting two nights ago. During that meeting, he sat with his head turned to the right for an extended period of time. As the meeting progressed, the pain in his neck gradually increased.
Analysis: When evaluating a patient complaining of upper posterior cervical pain, a number of conditions should be considered. These include:
• Upper cervical vertebral motion segment dysfunction
• Local muscle strain (e.g. suboccipital and upper trapezius muscles)
• Trapezius myofascial pain syndrome
• Upper cervical joint sprain
• Osteoarthritis
• Inflammatory arthritis
This is an acute presentation and the onset of the pain suggests a mechanical cause. However, practitioners should always be wary of other causes of pain including serious conditions such as fractures, infections and tumors.
What are the pain characteristics?
What are the aggravating and relieving factors?
What has been the course of the pain?
He describes his neck pain as a constant ache and rates it as a 4 out of 10 in intensity. He says that if he suddenly turns his neck to the right, the pain becomes sharp and rises to an 8 out of 10 in intensity. The neck pain worsens if he sits with his neck in a flexed position for an extended period of time. It improves immediately following a hot shower, but the pain soon returns. He says that the pain became worse the day after the onset but the intensity has not changed since.
Analysis: The pain characteristics as well as aggravating and relieving factors all support a mechanical cause. That the pain intensity has remained constant suggests the presence of local inflammation.
Are there any associated symptoms?
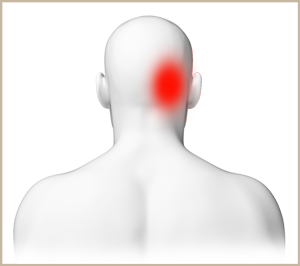
He describes his neck pain as his main concern. However, since the onset, he has also had a mild headache in the right occipital, periorbital, temporal and frontal regions. He also experiences tightness in the right suboccipital region.
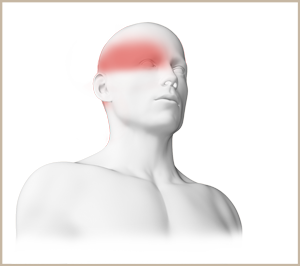
Analysis: When neck pain is accompanied by a headache, a number of possibilities should be considered to explain the complete presentation. In this patient, the location of the headache correlates with a pain referral pattern that is associated with upper cervical spine involvement. It also corresponds to pain referral patterns associated with myofascial pain syndrome such as that of the trapezius muscle.
Is there a past history that is relevant to the current complaint?
A review of his past history reveals a motor vehicle accident which happened 5 years ago in which his car collided with a stationary vehicle. This caused significant neck pain and stiffness that lasted for several weeks. He saw a medical practitioner who prescribed painkillers and anti-inflammatory medication. He believes that his neck fully recovered from that injury, but notes that he has had occasional headaches since then which are similar to the pain pattern he is experiencing now.
Analysis: His past history of neck injury indicate that the possible damage caused by the original trauma may have lead to residual joint or muscle involvement. This raises the possibility of the development of joint laxity, myofascial pain syndromes, muscle dysfunction or secondary osteoarthritis involving the upper back and neck. His description of his recurrent headaches since the accident being similar to the current presentation strongly indicates a correlation between his previous injury and the present complaint.
Are there any “red flags”?
The patient is asked the following questions in order to identify any “red flags” that could indicate serious pathology. Even if the patient has already provided information in the case history that relates to these questions, it is recommended that they are readdressed to ensure a thorough exploration.
Have you ever had any seizures? “No.”
Have you been diagnosed with high blood pressure? “No.”
Have you experienced any confusion, memory loss, double vision, dizziness or change in mental status or personality? “No.”
Is your headache brought on or worsened by bending over or by physical exertion such as coughing, sneezing, straining or sexual activity? “No.”
Have you recently experienced any neck stiffness, fever, chills, night sweats or vomiting? “No”.
Are your headaches increasing in intensity or frequency? “No.”
Do your symptoms disappear, even for a short time? “Yes. The pain tends to disappear when I’m resting in bed and after a hot shower.”
Does the pain wake you up at night? “No.”
Do you feel weak in your arms or legs? “No.”
Have you lost any weight recently? “No.”
Do you have a history of cancer or HIV? “No.”
Analysis: None of the patient’s responses raise a “red flag”.
What is the list of possible causes for the patient’s complaint?
Based on the available history, the initial list of possible causes for the patient’s complaint includes:
• Upper vertebral motion segment dysfunction (particularly at the C2-C3 level)
• Trapezius myofascial pain syndrome
Reflection Point
Please stop and take a moment to consider whether the main requirements of an adequate and relevant patient history taking have been fulfilled. Are there any additional questions you would have asked and, if so, why?
Before the physical examination findings are presented below, please reflect on what physical examination procedures you would perform to adequately evaluate this patient.
Performing Physical Examination
In the sections below, you are provided with examples of physical examination findings for this patient. The material presents a systematic approach to performing a focused and relevant physical examination in order to narrow down the possible causes for the patient’s complaint. The material also provides ongoing clinical reasoning and analysis of the findings. As you read the following material, you are encouraged to identify whether the essential elements of physical examination have been adequately covered.
Vital Signs
His vital signs are within normal limits.
Analysis: It is always important to examine the patient’s vital signs to screen for general health and identify any underlying conditions such as an infection.
Inspection
The patient appears to be in good general health. Postural examination reveals a slight tilt of the head to the right.
Analysis: The slightly tilted head posture may indicate an underlying spinal abnormality or may simply suggest a muscle imbalance.
Range of Motion
An assessment of cervical active and passive ranges of motion reveals a mild loss of movement in all directions, particularly in flexion. In addition, both lateral flexion and rotation to the right cause an increase in suboccipital discomfort.
Analysis: The loss of global active and passive ranges of motion typically suggests joint involvement. The suboccipital discomfort experienced on lateral flexion and rotation to the right suggests local muscle hypertonicity or joint involvement.
Palpation
Mild tenderness is reported in the middle of the belly of the upper trapezius with no nodularity or pain referral. Deeper palpation reveals mild tenderness over the suboccipital muscles on the right. An area of exquisite tenderness is detected over the right articular pillar at the C2-C3 level. With sustained pressure over this region, the patient reports a worsening of his headache. A functional examination of the vertebral motion segments is performed and reveals reduced movement at the C2-C3 vertebral level.
Analysis: The lack of nodularity or pain referral on palpation of the trapezius helps to rule out myofascial pain syndrome of that muscle. Tenderness on palpation of the right suboccipital muscles suggests their involvement. Palpation of the C2-C3 level and functional findings implicate the facet joints as the origin of the patient’s clinical presentation.
Neurological Examination
Given that the patient has presented with a headache, a neurological screening examination of the cranial nerves is performed. It is found to be normal.
Analysis: The normal results help to reinforce a mechanical cause for the patient’s presentation. Please watch the video below if you wish to view how a neurological screening examination of the cranial nerves is performed.
Reflection Point
Given the patient’s history and examination findings up until this point, please stop and take a moment to consider which special tests should be performed to further evaluate this patient.
Special Tests
Considering the clinical findings at this stage of the examination, a number of special tests are indicated. The Axial Cervical Compression test is performed and results in an increase in pain in the right upper cervical region. It also causes an aggravation of the patient’s headache.
Analysis: The results of this test suggest an involvement of the upper cervical facet joints. Please watch the video below if you wish to view how the Axial Cervical Compression test is performed.
The Cervical Distraction test is performed and this also results in an increase in pain in the right upper cervical region.
Analysis: The results of this test reinforces the involvement of the capsules of the upper cervical facet joints. Please watch the video below if you wish to view how the Cervical Distraction test is performed.
Reflection Point
Please stop and take a moment to consider whether all the elements of an adequate and relevant physical examination have been completed for this patient. Are there any additional procedures you would have performed and, if so, why?
Imaging
Plain radiographs of the cervical spine reveal mild intervertebral disc space narrowing and minimal osteophytosis in the mid to lower cervical region.
Diagnosis
C2-C3 facet joint dysfunction together with a cervicogenic headache
Discussion
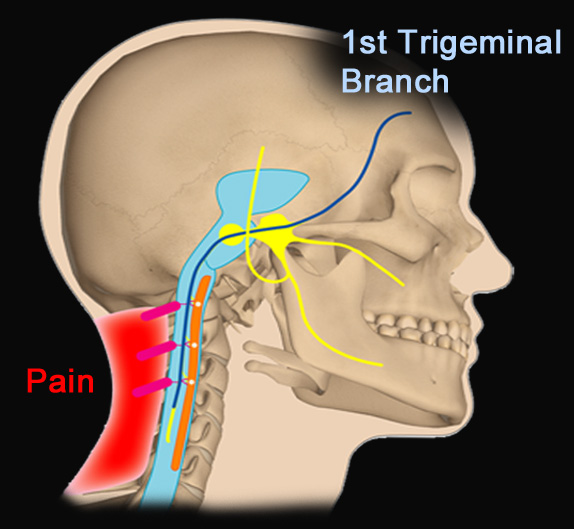
When patients present with neck pain and headache, cervicogenic causes need to be considered. It has been postulated that the pathophysiology of a cervicogenic headache relates to a neurological link that exists between the sensory fibers of the trigeminal nerve and the upper three cervical nerves. These nerves converge to form the trigeminocervical nucleus and create the anatomical basis whereby any musculoskeletal structures innervated by the C1 to C3 spinal nerves may be a source of a cervicogenic headache.
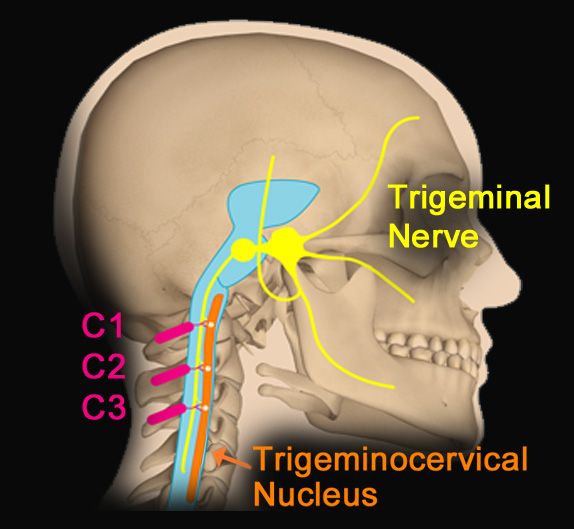
Musculoskeletal structures innervated by the C1 to C3 nerves include:
• The atlanto-occipital joints and ligaments
• The atlanto-axial (C1-C2) joints and ligaments
• The C2-C3 and the C3-C4 facet joints
• The C2-C3 intervertebral disc
• The suboccipital, upper cervical, trapezius and sternocleidomastoid muscles
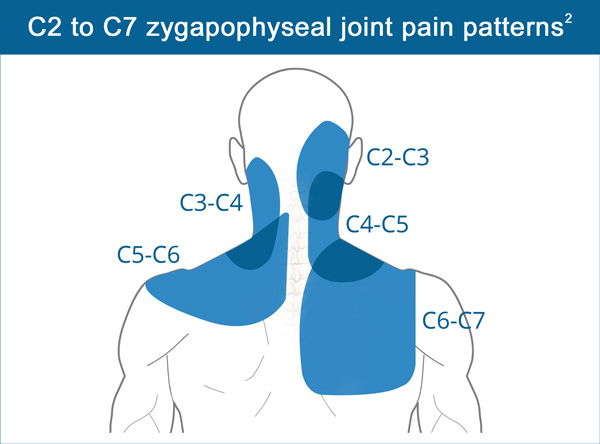
Involvement of the cervical facet joints can lead to localized neck pain or cause pain referral to the head, particularly the occiput, neck, shoulder and periscapular regions. Whilst these joints are likely to be injured in trauma such as “whiplash” injury, involvement can arise without the patient being able to recall a precipitating event. The cervical spine is also a region prone to the development of osteoarthritis, either secondary to a significant trauma or due to microtraumas accumulated over a lifetime.
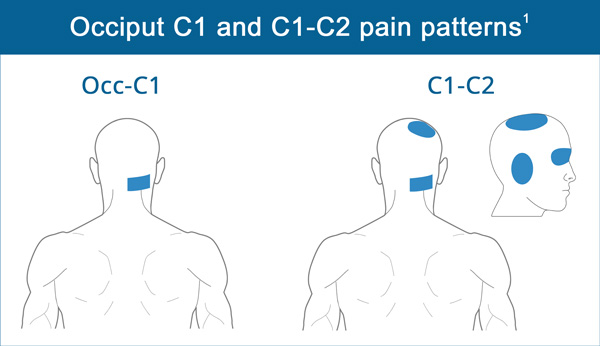
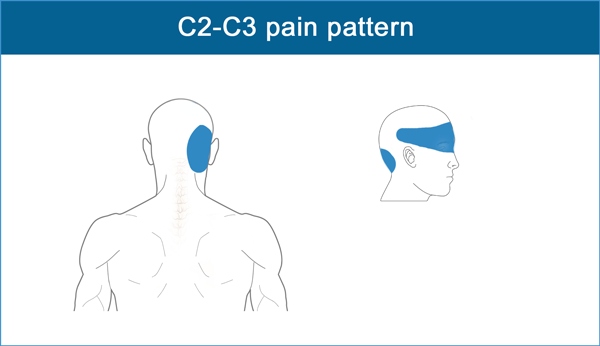
The location of referred pain may assist in determining the level and side of involvement. The following list provides a guide to the pain referral region for each of the cervical spine levels:
• Occ-C1: Occipital region
• C1-C2: Occiput, vertex, periorbital and periauricular
• C2-C3: Occiput, periorbital, temporal and frontal
• C3-C4: Upper and lateral neck
• C4-C5: Lateral neck from the base of the occiput to the base of the shoulder
• C5-C6: Lower neck and across the shoulder to the acromion
• C6-C7: Base of the neck, across the shoulder and the periscapular
It is suggested that the C2-C3 facet joint is the most frequent source of a cervicogenic headache. Involvement of the C1-C2 joint is likely the second most common source of a cervicogenic headache.
In whiplash injuries, the most frequent dysfunctional spinal segment causing headache is located at the C2-C3 level.
Convergence of the nerves in the trigeminocervical nucleus explains why functional disturbances of the upper cervical spine can lead to temporal or frontal head pain.
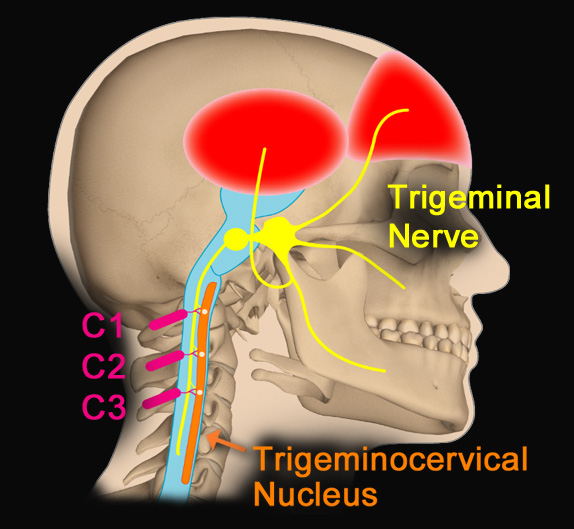
However, the convergence of the nerves in the trigeminocervical nucleus also explains the reverse situation. Pain originating from the first trigeminal branch can be experienced in the neck, as often seen in migraine patients.
Cervicogenic headaches can arise from a single trauma but may also occur as a result of repeated microtraumas, postural strain or poor ergonomics.
References and Suggested Further Readings:
Bogduk N, Govind J. Cervicogenic headache: an assessment of the evidence on clinical diagnosis, invasive tests and treatment. Lancet Neurol. 2009 Oct;8(10):959-68.
Dwyer A, Aprill C, Bogduk N. Cervical zygapophyseal joint pain patterns. I: A study in normal volunteers. Spine 1990 Jun;15(6):453-7.
Freeman M. Cervical Sprain and Strain. www.emedicine.medscape.com
Bajwa Z, Watson J. Cervicogenic headache. www.uptodate.com
Disclaimer: The Educom CE ™ website (including the text, graphics and videos that appear on the EducomCE.com) are designed to offer users general health information for educational purposes only. The general health information furnished on this site is not intended to replace personal consultation with a qualified healthcare professional. You must always seek the advice of a healthcare professional for questions related to your disease, disease symptoms, and appropriate therapeutic treatments.
Copyright © Educom Pty Ltd: All material on this website (including the text, graphics, videos and downloadable files) are owned by or licensed to Educom Pty Ltd and is subject to copyright and other intellectual property rights under international conventions.
