Case 3: Cholecystitis presenting as thoracolumbar pain (Preview)
Disclaimer: Please read the Disclaimer at the bottom of this page.
Copyright © Educom Pty Ltd: All material on this website (including the text, graphics, videos and downloadable files) are owned by or licensed to Educom Pty Ltd and is subject to copyright and other intellectual property rights under international conventions.
A Problem-Solving Approach to History Taking and Physical Examination
The learning material in this unit is designed to improve your skills in history taking and physical examination. The material includes examples of clinical findings and their analysis using a problem-solving approach. As you read through the material and watch the videos, you are encouraged to identify whether all the required elements of history taking and physical examination have been adequately covered.
Taking the Patient’s History
When taking the patient’s history, the practitioner needs to obtain sufficient information to cover the following essential elements:
• Who is the patient?
• Where is the pain?
• When was the onset?
• What caused the onset?
• What are the pain characteristics?
• What are the aggravating and relieving factors?
• What has been the course of the pain?
• Are there any associated symptoms?
• Is there a past history that is relevant to the current complaint?
• Are there any “red flags”?
• What is the list of possible causes for the patient’s complaint?
Who is the patient and where is the pain?
When was the onset and what caused the onset?
Your patient, a 31-year-old mother of two young children, presents with back pain. She points to the right lower posterior thorax as the site of her pain. The pain arose three days ago but she is unable to identify a cause.
Analysis: The location of the pain helps to narrow down the list of possible causes. They include:
• Lower thoracic to upper lumbar vertebral motion segment dysfunction
• Lower costovertebral joint dysfunction
• Local muscle strain (e.g., the erector spinae, serratus posterior inferior or intercostal muscles)
• Myofascial pain syndrome (e.g., the serratus posterior inferior or erector spinae muscles)
• Lower thoracic to upper lumbar disc herniation
As the patient is a mother with two young children, a mechanical cause for the pain is most likely. However, practitioners should always be wary of other causes of thoracic pain including serious conditions such as fractures, tumors and referred pain from visceral pathology (e.g., kidney or gallbladder disease).
What are the pain characteristics?
What are the aggravating and relieving factors?
What has been the course of the pain?
She describes the pain as a constant, deep and dull ache and rates it as a 6 out of 10 in intensity. She says that the movement of her torso in any direction worsens her pain and that it is particularly aggravated by bending backward and leaning to the right. In addition, deep inhalation and laughter significantly increase her pain. She is unable to identify any relieving factors. She says that the pain arose gradually and has increased since the onset to its current level.
Analysis: A deep aching pain can indicate joint inflammation, muscular disorders, bone pathology or visceral disease. Pain on movement in all directions, together with the aggravation caused by deep inhalation and laughter, typically suggests joint or bone pathology. That the patient is unable to identify a cause or any relieving factor requires consideration of an underlying pathology such as bone or visceral disease.
Are there any associated symptoms?
She says that she is not aware of any other symptoms.
Analysis: If a visceral disease were the underlying cause, we would have expected the patient to report symptoms of organ dysfunction (e.g., nausea, vomiting, fever, cough or dyspnoea). However, the absence of these associated symptoms does not necessarily rule out a visceral cause.
Is there a past history that is relevant to the current complaint?
The patient cannot recall having any pain in the same region in the past. She has, however, had a past history of low back pain in the lumbosacral and posterior pelvic regions. The most recent of these incidents occurred in the period immediately following the birth of her second child who is now 2 years old. She says that the quality of the pain that she experienced on those previous occasions was quite different to the pain that she is currently experiencing. Most notably, she was able to find relief with bed rest on those occasions, while her current pain is unrelenting.
Analysis: That the pain location and quality are new experiences for the patient and that this pain is unrelenting and without apparent cause, warrants consideration of an underlying non-mechanical pathology.
Are there any “red flags”?
The patient is asked the following questions in order to identify any “red flags” that could indicate serious pathology. Even if the patient has already provided information in the case history that relates to these questions, it is recommended that they are readdressed to ensure a thorough exploration.
Do your symptoms disappear, even for a short time? “No. The pain is unrelenting.”
Are your symptoms worsening? “Yes. As I said earlier, the pain is worsening.”
Does the pain wake you up at night? “The pain makes it very difficult for me to get to sleep, but I don’t think it causes me to wake up.”
Have you noticed any discoloration of your urine? “No.”
Have you had any bladder or bowel problems since the onset of your pain? “No.”
Do you feel weak in your arms or legs? “No.”
Have you recently experienced any fever, chills, night sweats or vomiting? “No.”
Have you lost any weight recently? “Yes. I have been dieting and exercising since the birth of my last child and have lost about 30 pounds.”
Do you have any breathing difficulties or a history of smoking? “No.”
Do you have diabetes? “No.”
Do you have a history of cancer or HIV? “No.”
Analysis: Both the unrelenting and worsening nature of her pain raise “red flags” and add to the concern already raised by her pain being in a new location, of a type not previously experienced and pain that is due to an unknown cause.
What is the list of possible causes for the patient’s complaint?
Based on the available history, the initial list of possible causes for the patient’s complaint includes:
• Visceral pathology (e.g., diseases of the kidney, gallbladder or lung)
• Bone pathology
• Joint pathology
• Spinal or costovertebral joint dysfunction
• Muscle strain (e.g., the erector spinae, serratus posterior inferior or intercostal muscles)
• Myofascial pain syndrome (e.g., the serratus posterior inferior or erector spinae muscles)
Reflection Point
Please stop and take a moment to consider whether the main requirements of an adequate and relevant patient history taking have been fulfilled. Are there any additional questions you would have asked and, if so, why?
Before the physical examination findings are presented below, please reflect on what physical examination procedures you would perform to adequately evaluate this patient.
Performing Physical Examination
In the sections below, you are provided with examples of physical examination findings for this patient. The material presents a systematic approach to performing a focused and relevant physical examination in order to narrow down the possible causes for the patient’s complaint. The material also provides ongoing clinical reasoning and analysis of the findings. As you read the following material, you are encouraged to identify whether the essential elements of physical examination have been adequately covered.
Vital Signs
Examination of the patient’s vital signs reveals a mild fever and mild tachycardia.
Analysis: These findings suggest the possibility of an underlying infection.
Inspection
Inspection reveals a mild prominence over the lower posterior thoracic cage on the right side. Otherwise, her postural evaluation is unremarkable.
Analysis: The mild prominence noted over the lower thoracic cage could indicate hypertonicity of the local musculature or an underlying skeletal deformity.
Range of Motion
Active and passive ranges of motion for the thoracolumbar spine are all moderately reduced as they cause an increase in her thoracolumbar pain. Extension and lateral flexion to the right are the most limited and the most provocative.
Analysis: A global loss of active and passive ranges of motion due to the exacerbation of thoracolumbar pain suggests spinal or costovertebral joint involvement. However, in light of the case history findings, pain arising from the distortion of nearby visceral structures cannot be ruled out.
Palpation
Palpation of the lower posterior thorax is performed with the patient in the prone position. It reveals local tenderness and an increase in muscle tone in the area of complaint. The patient reports that lying in the prone position is uncomfortable and that it causes a mild aggravation of her pain.
Analysis: The presence of tenderness and an increase in muscle tone indicate the presence of hypertonicity of the local musculature.
Neurological Examination
A neurological screening examination including assessment of the lower thoracic and lumbar dermatomes is normal except for a slight hyperalgesia over the right lower posterior thorax. The superficial abdominal reflexes in all quadrants are normal.
Analysis: Hyperalgesia is found in some neurological disorders but also in somatic and visceral referred pain patterns.
Abdominal Examination
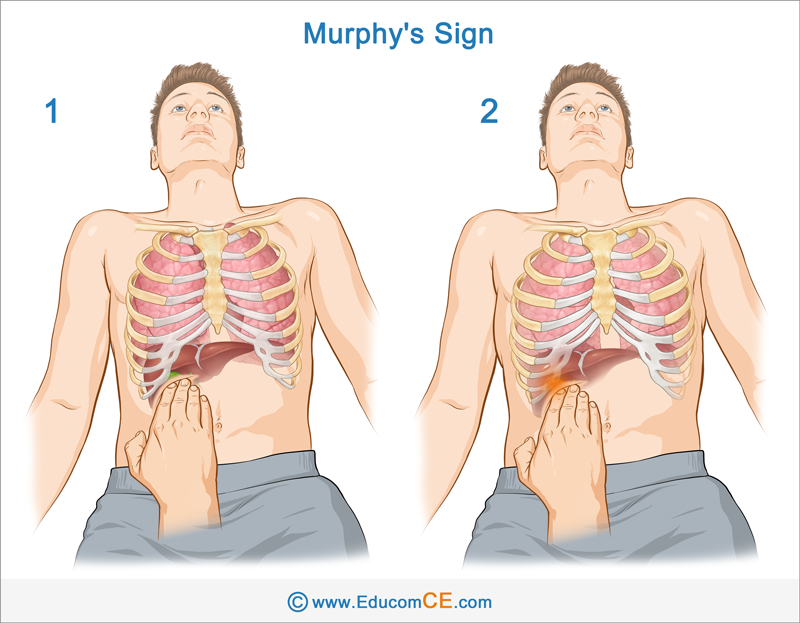
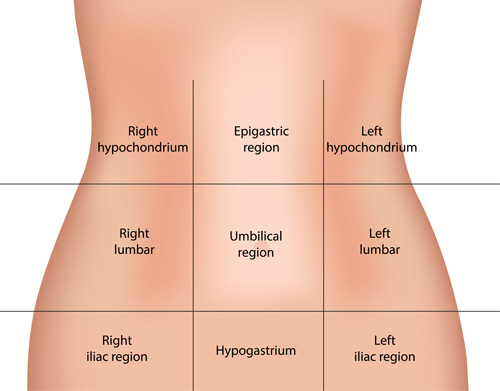
Palpation of the abdominal region reveals slight tenderness in the upper right quadrant, but the Murphy’s Sign is absent. The rest of the abdominal examination, including auscultation, is unremarkable.
Analysis: The presence of slight tenderness in the abdominal right upper quadrant may indicate liver or gallbladder involvement, even in the absence of the Murphy’s Sign (this Sign may not be present when the gallbladder involvement is in its mild stage).
Murphy’s Sign – The Murphys’ Sign is associated with gallbladder inflammation called cholecystitis. With the patient in the supine position, place your fingers below the right costal margin just medial to the mid-clavicular line. Ask the patient to exhale while you press your fingers up and under the costal margin. Now ask the patient to inhale deeply. This causes the gallbladder to descend and press against your fingers. Normally there is no pain and the patient is able to complete inhalation (Image 1). If the gallbladder is inflamed, the resulting pain will cause the patient to abruptly stop inhaling. This is called the Murphy’s Sign (Image 2).
Heart and Lung Examination
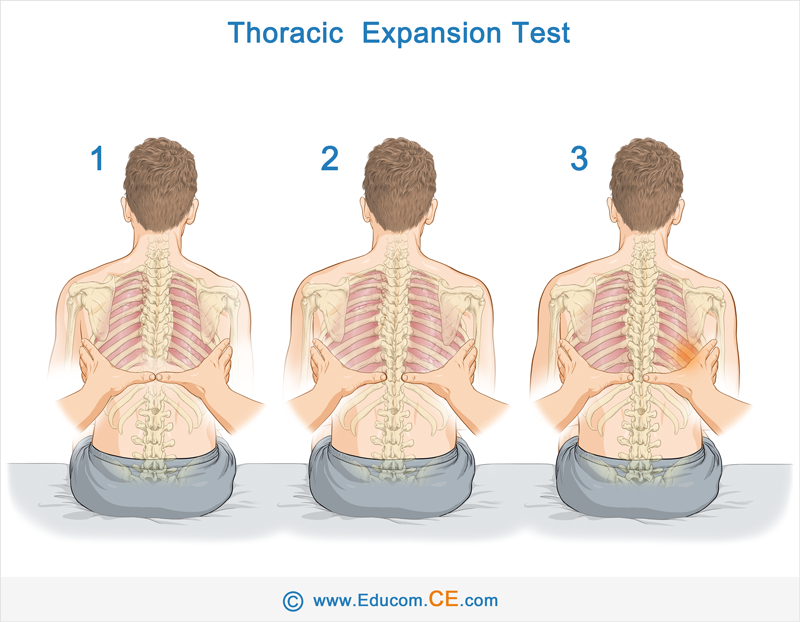
Examination of the heart and lungs is unremarkable except for the Thoracic Expansion test which results in an increase in the patient’s pain. However, the range of thoracic expansion is symmetrical and within normal limits.
Analysis: The normal findings of the heart and lung examination help to reduce the chance of their involvement. The Thoracic Expansion test is designed to detect the presence of lung pathology influencing the range of chest expansion. In this case, the test was within normal limits but the increase in pain that occurred could indicate either a mechanical involvement of the lower rib cage or a visceral irritation.
Thoracic Expansion Test – The Thoracic Expansion test measures the symmetry of thoracic cage movement. With the patient in the seated position, ask them to fully exhale. Now place your hands so that the thumbs touch at the level of the 10th ribs (Image 1). Ask the patient to take a deep breath in and hold it. Normally the thumbs should move in equal distance from the spine (Image 2). When there is an underlying unilateral lung pathology, the thumb on the involved side shows a reduced movement from the spine (Image 3).
Reflection Point
Given the patient’s history and examination findings up until this point, please stop and take a moment to consider which special tests should be performed to further evaluate this patient.
Special Test
The Lumbar Quadrant (Kemp’s) test is performed and causes an increase in pain in the right posterior lower thorax when performed with lateral flexion and extension on the right side.
Analysis: A positive Lumbar Quadrant test typically indicates the involvement of the zygapophyseal joints. However, in this patient, the findings could be explained by pain arising from the distortion of nearby visceral structures. Please watch the video below if you wish to view how the Lumbar Quadrant test is performed.
Reflection Point
Please stop and take a moment to consider whether all the elements of an adequate and relevant physical examination have been completed for this patient. Are there any additional procedures you would have performed and, if so, why?
Further Investigation
This patient has presented with a number of signs and symptoms of concern including:
• A new complaint in a new location
• Pain quality that has not been previously experienced
• Local right upper abdominal quadrant tenderness
• Local hyperalgesia
• Global loss of motion due to pain
• Mild fever and tachycardia
Given that these findings suggest the possibility of an underlying visceral disease, the patient is referred to her medical practitioner for further investigation. In a telephone conversation with the patient three days later, the patient reports that following the consumption of a fatty meal, she developed severe abdominal pain in the upper right quadrant and a significant increase in pain in her lower posterior thorax. A diagnostic ultrasound was performed later that day which confirmed a diagnosis of acute cholecystitis.
Diagnosis
Acute cholecystitis.
Please note: The above patient presentation has been adapted from a case report presented in the following journal article:
Carter C. Acute thoracolumbar pain due to cholecystitis: a case study. Chiropractic & Manual Therapies (2015) 23:34
Discussion
The following material is modified from the journal article referenced above.
The visceral pain of gallbladder origin – The majority of acute cholecystitis cases are due to the presence of cholelithiasis (gallstones). The production of gallstones and sludge at or near the neck of the gallbladder can cause obstruction of bile into the cystic duct, causing a number of pathophysiological nociception contributors that result in the production of visceral pain.
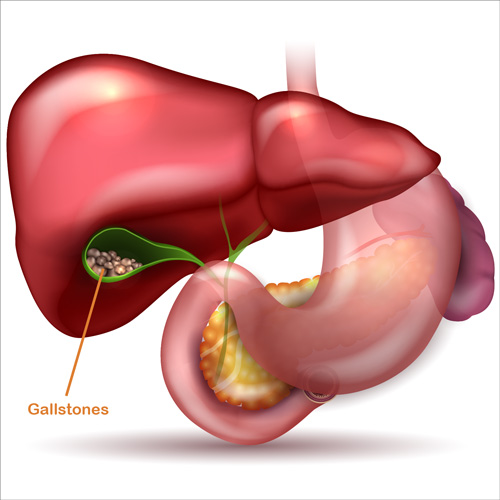
Once obstructed, the continued production of gallbladder mucus has no outlet for drainage and causes distension of the gallbladder wall and ducts. The subsequent increased peristalsis, which causes strong and sustained smooth muscle contraction, results in increased intraluminal pressure. This activation of gallbladder nociceptors by distension can occur in the absence of visceral inflammation and may present clinically as episodic biliary colic.
Nociceptor afferents from the gallbladder are carried anatomically via vagal and splanchnic nerves. However, the majority of nociception travels through the latter with their central terminations in dorsal and ventral horns of the spinal cord extending from T5 to L2. Therefore, the anatomical area of visceral pain perceived in acute cholecystitis significantly varies depending on which spinal segment second-order neurons are stimulated over such a broad spinal cord distribution.
Visceral pain is characterized as sharp, cramping or achy, although it tends to be diffuse, poorly localized and perceived deep inside. This is due to the relative paucity of peripheral afferent nociceptor terminals in the viscera, central terminal arborization, the distinct absence of a separate visceral sensory pathway, and overall low proportion of visceral afferent nociceptors compared with those of somatic origin.
Referred pain is commonly perceived in cholecystitis and can be an important clinical diagnostic measure. The occurrence of referred pain is best explained by the convergence-projection model which postulates that the majority of dorsal horn second-order neurons that receive afferent nociceptive input from the viscera also happen to receive input from somatic structures that share the same neuromeric field. In cholecystitis, referred pain to the back is explained by the dual synapsing of gallbladder afferents on the same viscerosomatic second-order neurons in the spinal cord that also receive innervation from somatic afferents coming from the right lower thoracic spine and ribs. The convergence-projection model also involves overlapping visceral and somatic nociception signaling to similar higher brain centers involved in the perception of pain, however the brain likely attributes the origin of the sensation to the somatic domain because of pneumonic traces of previously experienced somatic pain.
Muscle hypertonicity is a common finding in many mechanical musculoskeletal disorders. However, strong evidence exists for reflex efferent induced muscle contraction as a cause of the hyperalgesia seen in referred visceral pain syndromes. Muscle contraction is commonly seen in patients with acute visceral pain and has been histologically shown in rats to involve significant microscopic changes in muscle fiber phenotype. Referred pain to somatic structures is likely to involve not just central changes but also peripheral changes such as altered neurotransmitters and sensory terminals in the affected somatic tissue that affect tissue contractility.
The following summary of clinical manifestations in acute cholecystitis is referenced from www.uptodate.com:
Clinical History:
• Prolonged (more than four to six hours), steady, severe right upper quadrant or epigastric pain
• Referred pain may radiate to the right shoulder or back
• Fever, nausea, vomiting and anorexia
• Onset often follows the ingestion of fatty food
Physical Examination:
• Patient appears ill
• Elevated temperature and heart rate
• Abdominal pain aggravated by movement
• Abdominal guarding
• A positive Murphy’s Sign
References and Suggested Further Readings:
Carter C. Acute thoracolumbar pain due to cholecystitis: a case study. Chiropractic & Manual Therapies (2015) 23:34
Zakko S, Afdhal N. Acute cholecystitis: Pathogenesis, clinical features, and diagnosis. www.uptodate.com
Friedman G. Natural history of asymptomatic and symptomatic gallstones. Am J Surg. 1993 Apr;165(4):399-404.
Kalloo A, Kantsevoy S. Gallstones and biliary disease. Prim Care. 2001;28(3):591.
Bloom A. Cholecystitis. www. emedicine.medscape.com
Disclaimer: The Educom CE ™ website (including the text, graphics and videos that appear on the EducomCE.com) are designed to offer users general health information for educational purposes only. The general health information furnished on this site is not intended to replace personal consultation with a qualified healthcare professional. You must always seek the advice of a healthcare professional for questions related to your disease, disease symptoms, and appropriate therapeutic treatments.
Copyright © Educom Pty Ltd: All material on this website (including the text, graphics, videos and downloadable files) are owned by or licensed to Educom Pty Ltd and is subject to copyright and other intellectual property rights under international conventions.
