Case 2 – Cervical spondylotic myelopathy presenting as neck pain and paresthesia (Preview)
Disclaimer: Please read the Disclaimer at the bottom of this page.
Copyright © Educom Pty Ltd: All material on this website (including the text, graphics, videos and downloadable files) are owned by or licensed to Educom Pty Ltd and is subject to copyright and other intellectual property rights under international conventions.
A Problem-Solving Exercise in History Taking and Physical Examination
The learning material in this unit is designed to improve your skills in history taking and physical examination. The material includes examples of clinical findings and their analysis using a problem-solving approach. As you read through the material and watch the videos, you are encouraged to identify whether all the required elements of history taking and physical examination have been adequately covered.
Taking the Patient’s History
When taking the patient’s history, the practitioner needs to obtain sufficient information to cover the following essential elements:
• Who is the patient?
• Where is the pain?
• When was the onset?
• What caused the onset?
• What are the pain characteristics?
• What are the aggravating and relieving factors?
• What has been the course of the pain?
• Are there any associated symptoms?
• Is there a past history that is relevant to the current complaint?
• Are there any “red flags”?
• What is the list of possible causes for the patient’s complaint?
Who is the patient and where is the pain?
When was the onset and what caused the onset?
Your patient is a 76-year-old retired legal secretary who presents with pain and stiffness in her neck. She says that she has had these symptoms for many years but does not recall a specific cause.
Analysis: A number of conditions are found in older patients complaining of neck pain and stiffness including:
• Osteoarthritis
• Diffuse idiopathic skeletal hyperostosis
• Primary or secondary carcinoma
• Cervical vertebral motion segment dysfunction
• Muscle strain or Myofascial Pain Syndrome
In cases of older patients presenting with chronic neck pain and stiffness, disorders such as tumors need to also be considered..
What are the pain characteristics?
What are the aggravating and relieving factors?
What has been the course of the pain?
She describes her neck pain as an ache which varies in intensity. At its worst, she rates it as a 7 out of 10 in intensity. She reports that the symptoms are always worse in the morning but gradually improve during the day. However, if she undertakes too much activity her symptoms are aggravated and she needs to rest to get relief. She reports that both her neck pain and stiffness have been gradually worsening over the years.
Analysis: An aching type pain can indicate joint inflammation, muscular disorders or bone pathology. The pain rating indicates a moderate level of intensity. That her symptoms are worse in the morning and are relieved later is consistent with an arthritic condition. The return of symptoms with activity is also typical of an arthritic condition. The relief afforded by rest reinforces a mechanical cause for all of her symptoms. The gradual deterioration in her condition supports the presence of a degenerative disorder.
Are there any associated symptoms?
She reports a grating sensation when she moves her neck, particularly when rotating it to either side. She says that she sometimes experiences shooting pain down her arms and hands when she bends her neck forward. She reports that she has “strange sensations” in her arms and legs and says that it varies from tingling to numbness. She says that she is becoming increasingly clumsy and unsteady on her feet.
Analysis: The grating sensation felt on neck movement is often associated with a degenerative joint disease. The shooting pain in her upper extremities when she flexes her neck suggests spinal cord involvement. The sensory disturbances she describes, together with her apparent motor coordination difficulties, indicate neurological involvement. Their distribution into both the upper and lower extremities also suggests spinal cord involvement.
Is there a past history that is relevant to the current complaint?
She says that she had two car accidents when she was in her twenties, both of which resulted in neck pain. However, on each occasion, the pain resolved after a few weeks.
Analysis: The cervical trauma revealed in the patient’s history could have predisposed her to the development of cervical osteoarthritis.
Are there any “red flags”?
The patient is asked the following questions in order to identify any “red flags” that could indicate serious pathology. Even if the patient has already provided information in the case history that relates to these questions, it is recommended that they are readdressed to ensure a thorough exploration.
Do your symptoms disappear, even for a short time? “No, the pain doesn’t completely disappear. My neck pain and stiffness are usually much better by late morning, but the shooting pain into my arms can occur at any time.”
Does the pain wake you up at night? “No.”
Do you feel weak in your arms or legs? “Yes. I feel a loss of strength in my arms and hands. I seem to get tired quickly when I’m carrying my groceries.”
Have you recently experienced any fever, chills, night sweats or vomiting? “No.”
Have you lost any weight recently? “No.”
Do you have a history of cancer or HIV? “No.”
Analysis: Her reference to upper extremity weakness combined with her earlier reference to sensory disturbances, apparent motor coordination difficulties and the shooting pains she described on neck flexion constitute “red flags”.
What is the list of possible causes for the patient’s complaint?
Based on the available history, the initial list of possible causes for the patient’s complaint includes:
• Cervical myelopathy
• Widespread spinal degenerative joint disease with foraminal encroachment
• Central canal stenosis due to a space-occupying lesion or bone pathology
• Amyotrophic lateral sclerosis
• Multiple sclerosis
• Congenital canal stenosis
• Guillain-Barré syndrome
Reflection Point
Please stop and take a moment to consider whether the main requirements of an adequate and relevant patient history taking have been fulfilled. Are there any additional questions you would have asked and, if so, why?
Before the physical examination findings are presented below, please reflect on what physical examination procedures you would perform to adequately evaluate this patient.
Performing Physical Examination
In the sections below, you are provided with examples of physical examination findings for this patient. The material presents a systematic approach to performing a focused and relevant physical examination in order to narrow down the possible causes for the patient’s complaint. The material also provides ongoing clinical reasoning and analysis of the findings. As you read the following material, you are encouraged to identify whether the essential elements of physical examination have been adequately covered.
Vital Signs
Her vital signs are within normal limits.
Analysis: It is always important to examine a patient’s vital signs to screen for general health and identify any underlying conditions such as an infection.
Inspection
Postural examination reveals a mild hyperkyphosis in the thoracic region. She appears to avoid neck movement.
Analysis: The apparent limitation of cervical movement adds weight to the suspicion that the patient has osteoarthritis. The increased curve in the thoracic region may indicate osteoarthritis, poor muscle tone or the presence of osteopenia resulting in a compression fracture.
Range of Motion
Assessment of the cervical active and passive ranges of motion reveals a loss of movement in all directions. Rotation is limited to 45 degrees in either direction and is accompanied by crepitus. Flexion of the neck is limited and causes shooting pains in the upper limbs. Extension and lateral flexion of the neck are the least restricted.
Analysis: The global loss of ranges of motion is consistent with joint involvement. The crepitation on cervical rotation suggests degenerative joint disease. The shooting pain on flexion of the neck is known as the Lhermitte’s Sign and is considered to be a clinical finding associated with spinal cord involvement. To learn more about the Lhermitte’s Sign, please watch the video below.
Palpation
Palpation of the neck reveals tenderness over the spinous processes and articular pillars in the mid to lower cervical region. On deep palpation, the articular pillars feel nodular and prominent. Palpation of the muscles of the posterior cervical region reveals widespread tenderness.
Analysis: The tenderness on spinal palpation indicates an involvement of the cervical spine. The nodularity detected over the articular pillars may indicate osteophytosis involving the zygapophyseal joints. The tenderness of the posterior cervical musculature help to confirm the presence of a local musculoskeletal disorder which could include vertebral motion segment dysfunction, muscular dysfunction and osteoarthritis.
Neurological Examination
A neurological examination including an assessment of the C5 to T1 and L2-S1 nerve roots, the Romberg’s test and pathological reflex testing is performed and reveals the following:
• A loss of strength in wrist and finger flexion and wrist extension bilaterally
• A diffuse and patchy loss of sensation in the upper and lower extremities
• Decreased triceps reflexes bilaterally
• Decreased brachioradialis reflexes bilaterally
• Increased Achilles reflexes bilaterally
• The presence of the Hoffmann’s Reflex bilaterally
• The presence of the Babinski Response bilaterally
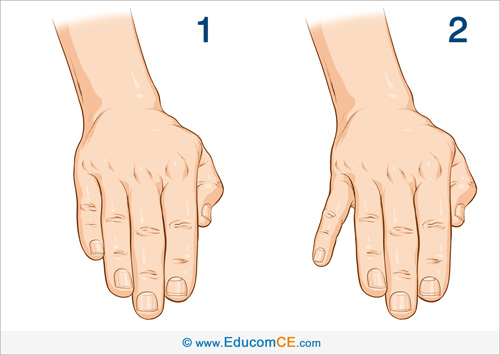
• The presence of the Finger Escape Sign bilaterally
• The presence of Ankle Clonus bilaterally
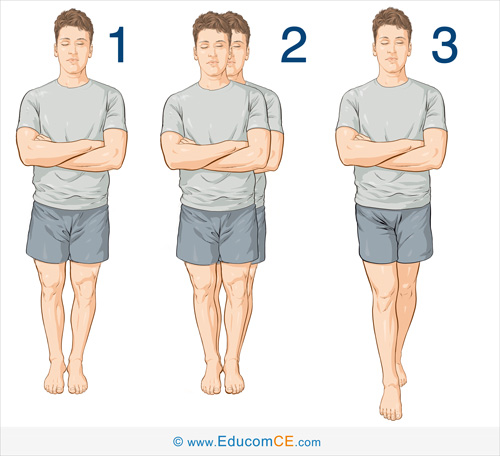
• A positive Romberg test
Analysis: The neurological examination findings are consistent with a combination of nerve root and spinal cord involvement. Please watch the videos below if you wish to view how these examination procedures are performed.
Finger Escape Sign: The Finger Escape Sign may be observed in patients with cervical myelopathy. Ask the patient to extend and adduct their fingers and maintain that position for up to a minute (Image 1). This test is considered positive if the small finger drifts into abduction (Image 2).
Romberg Test: The Romberg Test is used to detect a disturbance of proprioception. Ask the patient to stand with their feet together and their arms folded across their chest. Remain close at hand in case the patient begins to fall. Normally, the patient should be able to maintain this position with little or no swaying.
Now, ask the patient to close their eyes (Image 1). The patient should be able to maintain this position with only a small increase in swaying. If the patient sways excessively or begins to fall (Image 2), it is considered a positive Romberg’s test, indicating a problem with proprioception either from peripheral neuropathy or disease of the posterior columns.
Sharpened Romberg Test: To test for a more subtle deficiency of proprioception, a variation called the Sharpened Romberg Test can be performed. This test is also called the Tandem Romberg test. In this variation, the test is performed with the patient standing heel to toe (Image 3).
Reflection Point
Given the patient’s history and examination findings up until this point, please stop and take a moment to consider which special tests should be performed to further evaluate this patient.
Special Tests
In light of the case presentation thus far, it is thought that the performance of special provocative spinal tests may cause harm. Therefore, the patient is referred for imaging instead.
Reflection Point
Please stop and take a moment to consider whether all the elements of an adequate and relevant physical examination have been completed for this patient. Are there any additional procedures you would have performed, and if so, why?
Imaging
Plain radiographs of the cervical spine demonstrate moderate to severe osteoarthritis in the lower cervical spine. There is significant disc space narrowing and osteophytosis from C5 to T1, resulting in spinal stenosis at those levels. The intervertebral foramina at those levels are also significantly narrowed.
The patient is referred for magnetic resonance imaging of the cervical spine which reveals spondylotic cord compression in the lower cervical spine.
Diagnosis
Cervical spondylotic myelopathy of the lower cervical spinal cord and bilateral C6, C7 and C8 radiculopathy due to foraminal encroachment.
Discussion
Cervical spondylotic myelopathy is cervical spinal cord compression arising from spinal canal stenosis which was developed as a result of cervical spondylosis. Cervical spondylotic myelopathy is typically found in elderly patients and creates a variable clinical presentation involving upper and lower motor neuron involvement.
Signs and symptoms usually arise insidiously, with gait disturbance often the earliest finding. Any abrupt onset or exacerbation of symptoms warrants immediate referral for emergency medical investigation and attention. Neck trauma, such as that associated with a car accident, in the presence of significant spondylosis has the potential to develop into an acute onset of cervical myelopathy.
Signs and symptoms of cervical spondylotic myelopathy include:
• Neck pain
• Neck stiffness
• Pain in the shoulders, upper torso or arms
• Diffuse paresthesias that are dermatomal or non-dermatomal in distribution
• Muscle weakness
• Bladder retention, urination urgency or frequency
• Presence of the Finger Escape Sign and other variable muscle weakness
• Hyporeflexia (due to nerve root compression), muscle atrophy and weakness (most typically of C5 to C7 myotomes)
• Hyperreflexia (due to spinal cord compression)
• Loss of proprioception (posterior columns)
• A decrease in pain sensation (ventral spinothalamic tract)
• Presence of the Hoffmann’s Sign and the Babinski Response
• Lower extremity spasticity and clonus
• Gait disturbance (inability to perform toe-to-heel walking)
• A positive Romberg Test
• Presence of the Lhermitte’s Sign
References and Suggested Further Readings:
Fehlings MG, Skaf G. A review of the pathophysiology of cervical spondylotic myelopathy with insights for potential novel mechanisms drawn from traumatic spinal cord injury. Spine. 1998;23:2730–7.
McCormick WE, Steinmetz MP, Benzel EC. Cervical spondylotic myelopathy: make the difficult diagnosis, then refer for surgery. Cleve Clin J Med. 2003;70(10):899.
Sadasivan KK, Reddy RP, Albright JA. The natural history of cervical spondylotic myelopathy. Yale J Biol Med. 1993;66(3):235.
www.uptodate.com
Disclaimer: The Educom CE ™ website (including the text, graphics and videos that appear on the EducomCE.com) are designed to offer users general health information for educational purposes only. The general health information furnished on this site is not intended to replace personal consultation with a qualified healthcare professional. You must always seek the advice of a healthcare professional for questions related to your disease, disease symptoms, and appropriate therapeutic treatments.
Copyright © Educom Pty Ltd: All material on this website (including the text, graphics, videos and downloadable files) are owned by or licensed to Educom Pty Ltd and is subject to copyright and other intellectual property rights under international conventions.
